Scientific Resources
-
 文献Thacker SG et al. (OCT 2010) Journal of immunology (Baltimore,Md. : 1950) 185 7 4457--69
文献Thacker SG et al. (OCT 2010) Journal of immunology (Baltimore,Md. : 1950) 185 7 4457--69The detrimental effects of IFN-α on vasculogenesis in lupus are mediated by repression of IL-1 pathways: potential role in atherogenesis and renal vascular rarefaction.
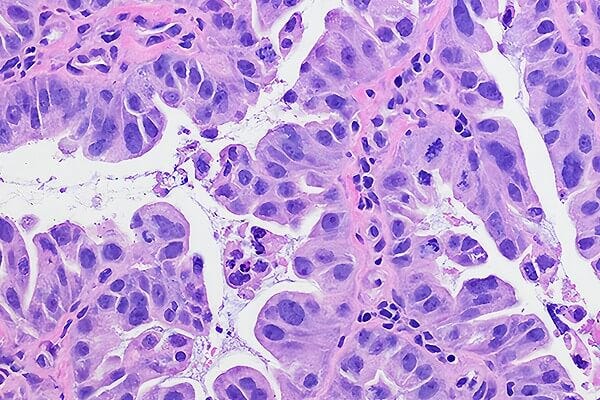
Systemic lupus erythematosus (SLE) is characterized by increased vascular risk due to premature atherosclerosis independent of traditional risk factors. We previously proposed that IFN-α plays a crucial role in premature vascular damage in SLE. IFN-α alters the balance between endothelial cell apoptosis and vascular repair mediated by endothelial progenitor cells (EPCs) and myeloid circulating angiogenic cells (CACs). In this study,we demonstrate that IFN-α promotes an antiangiogenic signature in SLE and control EPCs/CACs,characterized by transcriptional repression of IL-1α and β,IL-1R1,and vascular endothelial growth factor A,and upregulation of IL-1R antagonist and the decoy receptor IL-1R2. IL-1β promotes significant improvement in the functional capacity of lupus EPCs/CACs,therefore abrogating the deleterious effects of IFN-α. The beneficial effects from IL-1 are mediated,at least in part,by increases in EPC/CAC proliferation,by decreases in EPC/CAC apoptosis,and by preventing the skewing of CACs toward nonangiogenic pathways. IFN-α induces STAT2 and 6 phosphorylation in EPCs/CACs,and JAK inhibition abrogates the transcriptional antiangiogenic changes induced by IFN-α in these cells. Immunohistochemistry of renal biopsies from patients with lupus nephritis,but not anti-neutrophil cytoplasmic Ab-positive vasculitis,showed this pathway to be operational in vivo,with increased IL-1R antagonist,downregulation of vascular endothelial growth factor A,and glomerular and blood vessel decreased capillary density,compared with controls. Our study introduces a novel putative pathway by which type I IFNs may interfere with vascular repair in SLE through repression of IL-1-dependent pathways. This could promote atherosclerosis and loss of renal function in this disease. View Publication -
 文献Balasubramaniam V et al. (MAR 2010) American journal of physiology. Lung cellular and molecular physiology 298 3 L315--23
文献Balasubramaniam V et al. (MAR 2010) American journal of physiology. Lung cellular and molecular physiology 298 3 L315--23Bone marrow-derived angiogenic cells restore lung alveolar and vascular structure after neonatal hyperoxia in infant mice.
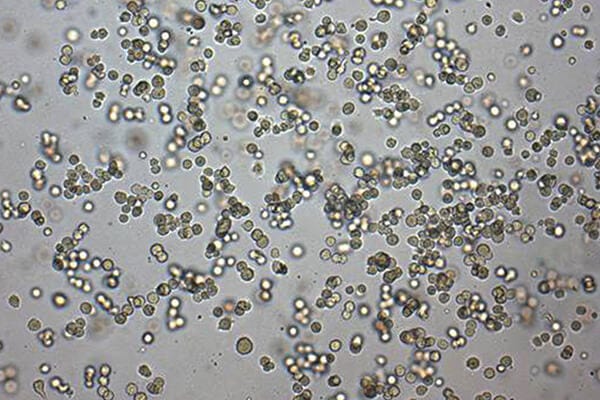
Neonatal hyperoxia impairs vascular and alveolar growth in mice and decreases endothelial progenitor cells. To determine the role of bone marrow-derived cells in restoration of neonatal lung structure after injury,we studied a novel bone marrow myeloid progenitor cell population from Tie2-green fluorescent protein (GFP) transgenic mice (bone marrow-derived angiogenic cells; BMDAC). We hypothesized that treatment with BMDAC would restore normal lung structure in infant mice during recovery from neonatal hyperoxia. Neonatal mice (1-day-old) were exposed to 80% oxygen for 10 days. BMDACs (1 x 10(5)),embryonic endothelial progenitor cells,mouse embryonic fibroblasts (control),or saline were then injected into the pulmonary circulation. At 21 days of age,saline-treated mice had enlarged alveoli,reduced septation,and a reduction in vascular density. In contrast,mice treated with BMDAC had complete restoration of lung structure that was indistinguishable from room air controls. BMDAC comprised 12% of distal lung cells localized to pulmonary vessels or alveolar type II (AT2) cells and persist (8.8%) for 8 wk postinjection. Coculture of AT2 cells or lung endothelial cells (luEC) with BMDAC augmented AT2 and luEC cell growth in vitro. We conclude that treatment with BMDAC after neonatal hyperoxia restores lung structure in this model of bronchopulmonary dysplasia. View Publication -
 文献Bruserud &O et al. (MAR 2007) Haematologica 92 3 332--41
文献Bruserud &O et al. (MAR 2007) Haematologica 92 3 332--41Subclassification of patients with acute myelogenous leukemia based on chemokine responsiveness and constitutive chemokine release by their leukemic cells.
BACKGROUND AND OBJECTIVES: Chemokines are soluble mediators involved in angiogenesis,cellular growth control and immunomodulation. In the present study we investigated the effects of various chemokines on proliferation of acute myelogenous leukemia (AML) cells and constitutive chemokine release by primary AML cells. DESIGN AND METHODS: Native human AML cells derived from 68 consecutive patients were cultured in vitro. We investigated AML cell proliferation (3H-thymidine incorporation,colony formation),chemokine receptor expression,constitutive chemokine release and chemotaxis of normal peripheral blood mononuclear cells. RESULTS: Exogenous chemokines usually did not have any effect on AML blast proliferation in the absence of hematopoietic growth factors,but when investigating growth factor-dependent (interleukin 3 + granulocyte-macrophage colony-stimulating factor + stem cell factor) proliferation in suspension cultures the following patient subsets were identified: (i) patients whose cells showed chemokine-induced growth enhancement (8 patients); (ii) divergent effects on proliferation (15 patients); and (iii) no effect (most patients). These patient subsets did not differ in chemokine receptor expression,but,compared to CD34- AML cells,CD34+ cells showed higher expression of several receptors. Chemokines also increased the proliferation of clonogenic AML cells from the first subset of patients. Furthermore,a broad constitutive chemokine release profile was detected for most patients,and the following chemokine clusters could be identified: CCL2-4/CXCL1/8,CCL5/CXCL9-11 (possibly also CCL23) and CCL13/17/22/24/CXCL5 (possibly also CXCL6). Only the CCL2-4/CXCL1/8 cluster showed significant correlations between corresponding mRNA levels and NFkB levels/activation. The chemotaxis of normal immunocompetent cells for patients without constitutive chemokine release was observed to be decreased. INTERPRETATION AND CONCLUSIONS: Differences in chemokine responsiveness as well as chemokine release contribute to patient heterogeneity in AML. Patients with AML can be classified into distinct subsets according to their chemokine responsiveness and chemokine release profile. View Publication -
 文献Maes C et al. (MAY 2006) The Journal of clinical investigation 116 5 1230--42
文献Maes C et al. (MAY 2006) The Journal of clinical investigation 116 5 1230--42Placental growth factor mediates mesenchymal cell development, cartilage turnover, and bone remodeling during fracture repair.
Current therapies for delayed- or nonunion bone fractures are still largely ineffective. Previous studies indicated that the VEGF homolog placental growth factor (PlGF) has a more significant role in disease than in health. Therefore we investigated the role of PlGF in a model of semi-stabilized bone fracture healing. Fracture repair in mice lacking PlGF was impaired and characterized by a massive accumulation of cartilage in the callus,reminiscent of delayed- or nonunion fractures. PlGF was required for the early recruitment of inflammatory cells and the vascularization of the fracture wound. Interestingly,however,PlGF also played a role in the subsequent stages of the repair process. Indeed in vivo and in vitro findings indicated that PlGF induced the proliferation and osteogenic differentiation of mesenchymal progenitors and stimulated cartilage turnover by particular MMPs. Later in the process,PlGF was required for the remodeling of the newly formed bone by stimulating osteoclast differentiation. As PlGF expression was increased throughout the process of bone repair and all the important cell types involved expressed its receptor VEGFR-1,the present data suggest that PlGF is required for mediating and coordinating the key aspects of fracture repair. Therefore PlGF may potentially offer therapeutic advantages for fracture repair. View Publication
过滤器
筛选结果
类别
- Product Information
Show More
Show Less
产品系列
- EasySep 1 项目
- MethoCult 3 项目
- StemSpan 2 项目
Show More
Show Less
资源类别
- 文献 4 项目
Show More
Show Less
细胞类型
- B 细胞 182 项目
- Cardiomyocytes 21 项目
- CD4+ 121 项目
- CD8+ 92 项目
- CHO细胞 3 项目
- Endoderm 18 项目
- Endothelial Cells 12 项目
- Epithelial Cells 29 项目
- HEK-293细胞(人胚肾293细胞) 1 项目
- Hematopoietic Cells 22 项目
- Hepatic Cells 13 项目
- HUVEC细胞(人脐静脉内皮细胞) 1 项目
- Mesenchymal Cells 18 项目
- Mesoderm 18 项目
- Neural Cells 89 项目
- NK 细胞 121 项目
- Other Subsets 21 项目
- PSC-Derived 128 项目
- PSC衍生 27 项目
- Regulatory 34 项目
- T Cells 102 项目
- T 细胞 352 项目
- 上皮细胞 106 项目
- 中胚层 1 项目
- 乳腺细胞 74 项目
- 先天性淋巴细胞 23 项目
- 全血 6 项目
- 内皮细胞 8 项目
- 内皮集落形成细胞(ECFCs) 3 项目
- 前列腺细胞 8 项目
- 单核细胞 142 项目
- 多巴胺能神经元 3 项目
- 多能干细胞 1859 项目
- 小胶质细胞 3 项目
- 巨噬细胞 25 项目
- 巨核细胞 8 项目
- 心肌细胞 15 项目
- 成骨细胞 6 项目
- 星形胶质细胞 2 项目
- 杂交瘤细胞 83 项目
- 树突状细胞(DCs) 91 项目
- 气道细胞 73 项目
- 淋巴细胞 33 项目
- 癌细胞及细胞系 130 项目
- 白细胞单采样本 12 项目
- 白血病/淋巴瘤细胞 14 项目
- 真皮细胞 2 项目
- 神经元 165 项目
- 神经干/祖细胞 420 项目
- 神经细胞 6 项目
- 粒细胞及其亚群 76 项目
- 红系细胞 9 项目
- 肌源干/祖细胞 9 项目
- 肝细胞 25 项目
- 肠道细胞 61 项目
- 肾细胞 3 项目
- 肾脏细胞 4 项目
- 肿瘤细胞 11 项目
- 胰腺细胞 12 项目
- 脂肪细胞 6 项目
- 脑肿瘤干细胞 87 项目
- 血小板 4 项目
- 血浆 16 项目
- 血管生成细胞 2 项目
- 调节性细胞 9 项目
- 软骨细胞 7 项目
- 造血干/祖细胞 874 项目
- 间充质基质细胞 13 项目
- 间充质干/祖细胞 156 项目
- 间充质细胞 1 项目
- 骨髓基质细胞 2 项目
- 骨髓瘤细胞 4 项目
- 髓系细胞 116 项目
- 鼠胚胎成纤维细胞 1 项目
- 白细胞 9 项目
- 其它细胞系 5 项目
- 红细胞 10 项目
Show More
Show Less
研究领域


 EasySep™小鼠TIL(CD45)正选试剂盒
EasySep™小鼠TIL(CD45)正选试剂盒



 沪公网安备31010102008431号
沪公网安备31010102008431号