Product Information
-
文献A. S. Smith et al. (jan 2022) Journal for immunotherapy of cancer 10 1
B cells imprint adoptively transferred CD8+ T cells with enhanced tumor immunity.
BACKGROUND Adoptive T cell transfer (ACT) therapy improves outcomes in patients with advanced malignancies,yet many individuals relapse due to the infusion of T cells with poor function or persistence. Toll-like receptor (TLR) agonists can invigorate antitumor T cell responses when administered directly to patients,but these responses often coincide with toxicities. We posited that TLR agonists could be repurposed ex vivo to condition T cells with remarkable potency in vivo,circumventing TLR-related toxicity. METHODS In this study we investigated how tumor-specific murine CD8+ T cells and human tumor infiltrating lymphocytes (TILs) are impacted when expanded ex vivo with the TLR9 agonist CpG. RESULTS Herein we reveal a new way to reverse the tolerant state of adoptively transferred CD8+ T cells against tumors using TLR-activated B cells. We repurposed the TLR9 agonist,CpG,commonly used in the clinic,to bolster T cell-B cell interactions during expansion for ACT. T cells expanded ex vivo from a CpG-treated culture demonstrated potent antitumor efficacy and prolonged persistence in vivo. This antitumor efficacy was accomplished without in vivo administration of TLR agonists or other adjuvants of high-dose interleukin (IL)-2 or vaccination,which are classically required for effective ACT therapy. CpG-conditioned CD8+ T cells acquired a unique proteomic signature hallmarked by an IL-2R$\alpha$highICOShighCD39low phenotype and an altered metabolic profile,all reliant on B cells transiently present in the culture. Likewise,human TILs benefitted from expansion with CpG ex vivo,as they also possessed the IL-2R$\alpha$highICOShighCD39low phenotype. CpG fostered the expansion of potent CD8+ T cells with the signature phenotype and antitumor ability via empowering a direct B-T cell interaction. Isolated B cells also imparted T cells with the CpG-associated phenotype and improved tumor immunity without the aid of additional antigen-presenting cells or other immune cells in the culture. CONCLUSIONS Our results demonstrate a novel way to use TLR agonists to improve immunotherapy and reveal a vital role for B cells in the generation of potent CD8+ T cell-based therapies. Our findings have immediate implications in the clinical treatment of advanced solid tumors. View Publication -
文献E. Xu et al. (jan 2022) Molecular neurodegeneration 17 1 7
Pathological $\alpha$-synuclein recruits LRRK2 expressing pro-inflammatory monocytes to the brain.
BACKGROUND Leucine rich repeat kinase 2 (LRRK2) and SNCA are genetically linked to late-onset Parkinson's disease (PD). Aggregated $\alpha$-synuclein pathologically defines PD. Recent studies identified elevated LRRK2 expression in pro-inflammatory CD16+ monocytes in idiopathic PD,as well as increased phosphorylation of the LRRK2 kinase substrate Rab10 in monocytes in some LRRK2 mutation carriers. Brain-engrafting pro-inflammatory monocytes have been implicated in dopaminergic neurodegeneration in PD models. Here we examine how $\alpha$-synuclein and LRRK2 interact in monocytes and subsequent neuroinflammatory responses. METHODS Human and mouse monocytes were differentiated to distinct transcriptional states resembling macrophages,dendritic cells,or microglia,and exposed to well-characterized human or mouse $\alpha$-synuclein fibrils. LRRK2 expression and LRRK2-dependent Rab10 phosphorylation were measured with monoclonal antibodies,and myeloid cell responses to $\alpha$-synuclein fibrils in R1441C-Lrrk2 knock-in mice or G2019S-Lrrk2 BAC mice were evaluated by flow cytometry. Chemotaxis assays were performed with monocyte-derived macrophages stimulated with $\alpha$-synuclein fibrils and microglia in Boyden chambers. RESULTS $\alpha$-synuclein fibrils robustly stimulate LRRK2 and Rab10 phosphorylation in human and mouse macrophages and dendritic-like cells. In these cells,$\alpha$-synuclein fibrils stimulate LRRK2 through JAK-STAT activation and intrinsic LRRK2 kinase activity in a feed-forward pathway that upregulates phosphorylated Rab10. In contrast,LRRK2 expression and Rab10 phosphorylation are both suppressed in microglia-like cells that are otherwise highly responsive to $\alpha$-synuclein fibrils. Corroborating these results,LRRK2 expression in the brain parenchyma occurs in pro-inflammatory monocytes infiltrating from the periphery,distinct from brain-resident microglia. Mice expressing pathogenic LRRK2 mutations G2019S or R1441C have increased numbers of infiltrating pro-inflammatory monocytes in acute response to $\alpha$-synuclein fibrils. In primary cultured macrophages,LRRK2 kinase inhibition dampens $\alpha$-synuclein fibril and microglia-stimulated chemotaxis. CONCLUSIONS Pathologic $\alpha$-synuclein activates LRRK2 expression and kinase activity in monocytes and induces their recruitment to the brain. These results predict that LRRK2 kinase inhibition may attenuate damaging pro-inflammatory monocyte responses in the brain. View Publication -
文献M. Kono et al. ( 2022) Oncoimmunology 11 1 2021619
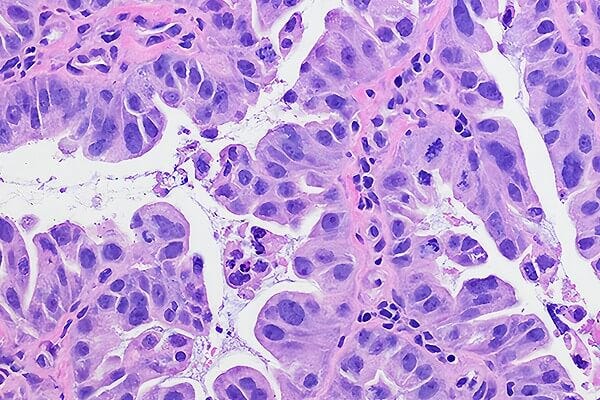
Immunomodulation via FGFR inhibition augments FGFR1 targeting T-cell based antitumor immunotherapy for head and neck squamous cell carcinoma.
Fibroblast growth factor receptor 1 (FGFR1) is overexpressed in multiple types of solid tumors,including head and neck squamous cell carcinoma (HNSCC). Being associated with poor prognosis,FGFR1 is a potential therapeutic target for aggressive tumors. T cell-based cancer immunotherapy has played a central role in novel cancer treatments. However,the potential of antitumor immunotherapy targeting FGFR1 has not been investigated. Here,we showed that FGFR-tyrosine kinase inhibitors (TKIs) augmented antitumor effects of immune checkpoint inhibitors in an HNSCC mouse model and upregulated tumoral MHC class I and MHC class II expression in vivo and in vitro. This upregulation was associated with the mitogen-activated protein kinase signaling pathway,which is a crucial pathway for cancer development through FGFR signaling. Moreover,we identified an FGFR1-derived peptide epitope (FGFR1305-319) that could elicit antigen-reactive and multiple HLA-restricted CD4+ T cell responses. These T cells showed direct cytotoxicity against tumor cells that expressed FGFR1. Notably,FGFR-TKIs augmented antitumor effects of FGFR1-reactive T cells against human HNSCC cells. These results indicate that the combination of FGFR-TKIs with immunotherapy,such as an FGFR1-targeting peptide vaccine or immune checkpoint inhibitor,could be a novel and robust immunologic approach for treating patients with FGFR1-expressing cancer cells. View Publication -
文献Y. Xia et al. ( 2021) Frontiers in pharmacology 12 746786
Yi Shen Juan Bi Pill Regulates the Bone Immune Microenvironment via the JAK2/STAT3 Signaling Pathway in Vitro.
Rheumatoid arthritis (RA) is characterized by an impaired articular bone immune microenvironment,which is associated with regulatory T cells (Tregs) hypofunction and osteoclasts (OCs) hyperfunction and leads to articular bone erosion and systemic bone loss. Studies have shown that Tregs slow bone loss in RA by regulating the bone resorption function of OCs and the JAK/STAT signaling pathway can regulate the immunosuppressive function of Tregs and reduce the bone erosion function of OCs. Yi Shen Juan Bi Pill (YSJB) is a classic Chinese herbal compound for the treatment of RA. However,whether YSJB regulates bone immune microenvironment homeostasis through JAK/STAT signaling pathway remains unclear. Based on in vitro OC single culture,Treg single culture and OC-Treg coculture systems,treatments were performed using drug-containing serum,AG490 and JAK2 siRNA to explore whether YSJB-containing serum regulates the homeostasis of the bone immune microenvironment through the JAK/STAT signaling pathway. In vitro,YSJB treatment decreased the number of TRAP+ cells and the areas of bone resorption and inhibited the expression of RANK,NFATc1,c-fos,JAK2,and STAT3 in both the OC single culture system and the OC-Treg coculture system. Tregs further reduced the number of TRAP+ cells and the areas of bone resorption in the coculture system. YSJB promoted the secretion of IL-10 while inhibiting the expression of JAK2 and STAT3 in Tregs. Moreover,inhibiting the expression of JAK2 with the JAK2 inhibitor AG490 and JAK2 siRNA improved the immunosuppressive functions of Treg,inhibited OC differentiation and bone resorption. Our study demonstrates that YSJB can regulate OC-mediated bone resorption and Treg-mediated bone immunity through the JAK2/STAT3 signaling pathway. This study provides a new strategy for regulating the bone immune microenvironment in RA with traditional Chinese medicine. View Publication -
文献T. P. Buters et al. (apr 2022) Clinical pharmacology and therapeutics 111 4 964--971
Clinical, Cellular, and Molecular Effects of Corticosteroids on the Response to Intradermal Lipopolysaccharide Administration in Healthy Volunteers.
The intradermal lipopolysaccharide (LPS) challenge in healthy volunteers has proven to be a valuable tool to study local inflammation in vivo. In the current study the inhibitory effects of oral and topical corticosteroid treatment on intradermal LPS responses were evaluated to benchmark the challenge for future investigational drugs. Twenty-four healthy male volunteers received a two-and-a-half-day twice daily (b.i.d.) pretreatment with topical clobetasol propionate 0.05% and six healthy volunteers received a two-and-a-half-day b.i.d. pretreatment with oral prednisolone at 0.25 mg/kg body weight per administration. Participants received one injection regimen of either 0,2,or 4 intradermal LPS injections (5 ng LPS in 50 µL 0.9% sodium chloride solution). The LPS response was evaluated by noninvasive (perfusion,skin temperature,and erythema) and invasive assessments (cellular and cytokine responses) in suction blister exudate. Both corticosteroids significantly suppressed the clinical inflammatory response (erythema P = 0.0001 for clobetasol and P = 0.0016 for prednisolone; heat P = 0.0245 for clobetasol,perfusion P < 0.0001 for clobetasol and P = 0.0036 for prednisolone). Clobetasol also significantly reduced the number of monocytes subsets,dendritic cells,natural killer cells,and T cells in blister exudate. A similar effect was observed for prednisolone. No relevant corticosteroid effects were observed on the cytokine response to LPS. We successfully demonstrated that the anti-inflammatory effects of corticosteroids can be detected using our intradermal LPS challenge model,validating it for evaluation of future investigational drugs,as an initial assessment of the anti-inflammatory effects of such compounds in a minimally invasive manner. View Publication -
文献F. Shahneh et al. (feb 2022) Arteriosclerosis,thrombosis,and vascular biology 42 2 145--155
Inflammatory Monocyte Counts Determine Venous Blood Clot Formation and Resolution.
BACKGROUND Monocytes are thought to be involved in venous thrombosis but the role of individual monocyte subpopulations on thrombus formation,clot inflammation,and degradation is an important unresolved issue. We investigate the role of inflammatory Ly6Chi monocytes in deep vein thrombosis and their potential therapeutic impact. METHODS Frequencies and compositions of blood monocytes were analyzed by flow cytometry in CCR2-/- (C-C chemokine receptor type 2) and wild-type mice of different ages and after treatment with the NR4A1 (nuclear receptor group 4 family A member 1,Nur77) agonist CnsB (cytosporone B). TF (tissue factor) sufficient and deficient Ly6Chi monocytes were adoptively transferred into aged CCR2-/- mice. Thrombus formation and size were followed by ultrasound over a 3-week period after surgical reduction of blood flow (stenosis) in the inferior vena cava. RESULTS Reduced numbers of peripheral monocytes in aged (>30 w) CCR2-/- mice are accompanied by reduced thrombus formation after inferior vena cava ligation. Reducing the number of inflammatory Ly6Chi monocytes in wild-type mice by CsnB treatment before ligation,similarly suspends clotting,while later treatment (d1 or d4) reduces thrombus growth and accelerates resolution. We describe how changes in inflammatory monocyte numbers affect the gradual differentiation of monocytes in thrombi and show that only tissue factor-competent Ly6Chi monocytes restore thrombosis in aged CCR2-/- mice. CONCLUSIONS We conclude that the number of inflammatory Ly6Chi monocytes controls deep vein thrombosis formation,growth,and resolution and can be therapeutically manipulated with a NR4A1 agonist at all disease stages. View Publication -
文献A. Xu et al. (jan 2022) Journal of immunology (Baltimore,Md. : 1950) 208 1 155--168
Prosurvival IL-7-Stimulated Weak Strength of mTORC1-S6K Controls T Cell Memory via Transcriptional FOXO1-TCF1-Id3 and Metabolic AMPK$\alpha$1-ULK1-ATG7 Pathways.
CD8+ memory T (TM) cells play a critical role in immune defense against infection. Two common $\gamma$-chain family cytokines,IL-2 and IL-7,although triggering the same mTORC1-S6K pathway,distinctly induce effector T (TE) cells and TM cells,respectively,but the underlying mechanism(s) remains elusive. In this study,we generated IL-7R-/and AMPK$\alpha$1-knockout (KO)/OTI mice. By using genetic and pharmaceutical tools,we demonstrate that IL-7 deficiency represses expression of FOXO1,TCF1,p-AMPK$\alpha$1 (T172),and p-ULK1 (S555) and abolishes T cell memory differentiation in IL-7R KO T cells after Listeria monocytogenesis rLmOVA infection. IL-2- and IL-7-stimulated strong and weak S6K (IL-2/S6Kstrong and IL-7/S6Kweak) signals control short-lived IL-7R-CD62L-KLRG1+ TE and long-term IL-7R+CD62L+KLRG1- TM cell formations,respectively. To assess underlying molecular pathway(s),we performed flow cytometry,Western blotting,confocal microscopy,and Seahorse assay analyses by using the IL-7/S6Kweak-stimulated TM (IL-7/TM) and the control IL-2/S6Kstrong-stimulated TE (IL-2/TE) cells. We determine that the IL-7/S6Kweak signal activates transcriptional FOXO1,TCF1,and Id3 and metabolic p-AMPK$\alpha$1,p-ULK1,and ATG7 molecules in IL-7/TM cells. IL-7/TM cells upregulate IL-7R and CD62L,promote mitochondria biogenesis and fatty acid oxidation metabolism,and show long-term cell survival and functional recall responses. Interestingly,AMPK$\alpha$1 deficiency abolishes the AMPK$\alpha$1 but maintains the FOXO1 pathway and induces a metabolic switch from fatty acid oxidation to glycolysis in AMPK$\alpha$1 KO IL-7/TM cells,leading to loss of cell survival and recall responses. Taken together,our data demonstrate that IL-7-stimulated weak strength of mTORC1-S6K signaling controls T cell memory via activation of transcriptional FOXO1-TCF1-Id3 and metabolic AMPK$\alpha$1-ULK1-ATG7 pathways. This (to our knowledge) novel finding provides a new mechanism for a distinct IL-2/IL-7 stimulation model in T cell memory and greatly impacts vaccine development. View Publication -
文献I. Gonz\'alez-Mariscal et al. (jan 2022) Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie 145 112361
Abnormal cannabidiol ameliorates inflammation preserving pancreatic beta cells in mouse models of experimental type 1 diabetes and beta cell damage.
The atypical cannabinoid Abn-CBD improves the inflammatory status in preclinical models of several pathologies,including autoimmune diseases. However,its potential for modulating inflammation in autoimmune type 1 diabetes (T1D) is unknown. Herein we investigate whether Abn-CBD can modulate the inflammatory response during T1D onset using a mouse model of T1D (non-obese diabetic- (NOD)-mice) and of beta cell damage (streptozotocin (STZ)-injected mice). Six-week-old female NOD mice were treated with Abn-CBD (0.1-1 mg/kg) or vehicle during 12 weeks and then euthanized. Eight-to-ten-week-old male C57Bl6/J mice were pre-treated with Abn-CBD (1 mg/kg of body weight) or vehicle for 1 week,following STZ challenge,and euthanized 1 week later. Blood,pancreas,pancreatic lymph nodes (PLNs) and T cells were collected and processed for analysis. Glycemia was also monitored. In NOD mice,treatment with Abn-CBD significantly reduced the severity of insulitis and reduced the pro-inflammatory profile of CD4+ T cells compared to vehicle. Concomitantly,Abn-CBD significantly reduced islet cell apoptosis and improved glucose tolerance. In STZ-injected mice,Abn-CBD decreased circulating proinflammatory cytokines and ameliorated islet inflammation reducing intra-islet phospho-NF-$\kappa$B and TXNIP. Abn-CBD significantly reduced 2 folds intra-islet CD8+ T cells and reduced Th1/non-Th1 ratio in PLNs of STZ-injected mice. Islet cell apoptosis and intra-islet fibrosis were also significantly reduced in Abn-CBD pre-treated mice compared to vehicle. Altogether,Abn-CBD reduces circulating and intra-islet inflammation,preserving islets,thus delaying the progression of insulitis. Hence,Abn-CBD and related compounds emerge as new candidates to develop pharmacological strategies to treat the early stages of T1D. View Publication -
文献M. Klopotowska et al. (feb 2022) Cancer immunology research 10 2 228--244
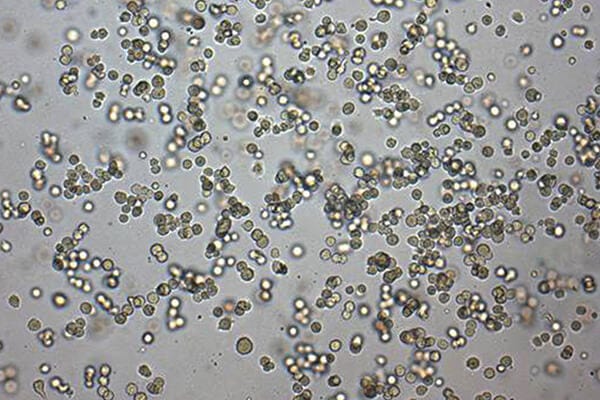
PRDX-1 Supports the Survival and Antitumor Activity of Primary and CAR-Modified NK Cells under Oxidative Stress.
Oxidative stress,caused by the imbalance between reactive species generation and the dysfunctional capacity of antioxidant defenses,is one of the characteristic features of cancer. Here,we quantified hydrogen peroxide in the tumor microenvironment (TME) and demonstrated that hydrogen peroxide concentrations are elevated in tumor interstitial fluid isolated from murine breast cancers in vivo,when compared with blood or normal subcutaneous fluid. Therefore,we investigated the effects of increased hydrogen peroxide concentration on immune cell functions. NK cells were more susceptible to hydrogen peroxide than T cells or B cells,and by comparing T,B,and NK cells' sensitivities to redox stress and their antioxidant capacities,we identified peroxiredoxin-1 (PRDX1) as a lacking element of NK cells' antioxidative defense. We observed that priming with IL15 protected NK cells' functions in the presence of high hydrogen peroxide and simultaneously upregulated PRDX1 expression. However,the effect of IL15 on PRDX1 expression was transient and strictly dependent on the presence of the cytokine. Therefore,we genetically modified NK cells to stably overexpress PRDX1,which led to increased survival and NK cell activity in redox stress conditions. Finally,we generated PD-L1-CAR NK cells overexpressing PRDX1 that displayed potent antitumor activity against breast cancer cells under oxidative stress. These results demonstrate that hydrogen peroxide,at concentrations detected in the TME,suppresses NK cell function and that genetic modification strategies can improve CAR NK cells' resistance and potency against solid tumors. View Publication -
文献A. K. Jaiswal et al. (jan 2022) American journal of physiology. Lung cellular and molecular physiology 322 1 L102--L115
Short palate, lung, and nasal epithelial clone 1 (SPLUNC1) level determines steroid-resistant airway inflammation in aging.
Asthma and its heterogeneity change with age. Increased airspace neutrophil numbers contribute to severe steroid-resistant asthma exacerbation in the elderly,which correlates with the changes seen in adults with asthma. However,whether that resembles the same disease mechanism and pathophysiology in aged and adults is poorly understood. Here,we sought to address the underlying molecular mechanism of steroid-resistant airway inflammation development and response to corticosteroid (Dex) therapy in aged mice. To study the changes in inflammatory mechanism,we used a clinically relevant treatment model of house-dust mite (HDM)-induced allergic asthma and investigated lung adaptive immune response in adult (20-22 wk old) and aged (80-82 wk old) mice. Our result indicates an age-dependent increase in airway hyperresponsiveness (AHR),mixed granulomatous airway inflammation comprising eosinophils and neutrophils,and Th1/Th17 immune response with progressive decrease in frequencies and numbers of HDM-bearing dendritic cells (DC) accumulation in the draining lymph node (DLn) of aged mice as compared with adult mice. RNA-Seq experiments of the aged lung revealed short palate,lung,and nasal epithelial clone 1 (SPLUNC1) as one of the steroid-responsive genes,which progressively declined with age and further by HDM-induced inflammation. Moreover,we found increased glycolytic reprogramming,maturation/activation of DCs,the proliferation of OT-II cells,and Th2 cytokine secretion with recombinant SPLUNC1 (rSPLUNC1) treatment. Our results indicate a novel immunomodulatory role of SPLUNC1 regulating metabolic adaptation/maturation of DC. An age-dependent decline in the SPLUNC1 level may be involved in developing steroid-resistant airway inflammation and asthma heterogeneity. View Publication
过滤器
筛选结果
类别
- References
- Safety Data Sheets
- Technical Manuals
- Product Information Sheets
- Special Protocols
Show More
Show Less
产品类型
产品系列
- ALDECOUNT 7 项目
- CellPore 1 项目
- EasyPick 2 项目
- ES-Cult 78 项目
- iCell 3 项目
- MegaCult 35 项目
- ALDEFLUOR 223 项目
- AggreWell 56 项目
- BrainPhys 31 项目
- ClonaCell 85 项目
- CryoStor 66 项目
- EasySep 625 项目
- EpiCult 12 项目
- ImmunoCult 1 项目
- IntestiCult 73 项目
- Lymphoprep 14 项目
- MammoCult 50 项目
- MesenCult 86 项目
- MethoCult 482 项目
- MyeloCult 76 项目
- NeuroCult 349 项目
- NeuroFluor 1 项目
- PancreaCult 2 项目
- PneumaCult 45 项目
- RSeT 8 项目
- RoboSep 59 项目
- RosetteSep 252 项目
- STEMdiff 44 项目
- STEMvision 8 项目
- SepMate 25 项目
- StemSpan 287 项目
- TeSR 1581 项目
- ThawSTAR 1 项目
- mFreSR 14 项目
Show More
Show Less
资源类别
- 产品信息表 5316 项目
- 协议 1 项目
- 安全数据表 4600 项目
- 技术手册 82 项目
- 文献 5873 项目
Show More
Show Less
细胞类型
- B 细胞 134 项目
- CD4+ 84 项目
- CD8+ 48 项目
- Endoderm 1 项目
- Neural Cells 17 项目
- NK 细胞 79 项目
- PSC-Derived 18 项目
- PSC衍生 6 项目
- Regulatory 11 项目
- T Cells 56 项目
- T 细胞 252 项目
- 上皮细胞 47 项目
- 乳腺细胞 68 项目
- 先天性淋巴细胞 3 项目
- 内皮细胞 2 项目
- 前列腺细胞 7 项目
- 单核细胞 106 项目
- 多能干细胞 1692 项目
- 心肌细胞 3 项目
- 杂交瘤细胞 76 项目
- 树突状细胞(DCs) 59 项目
- 气道细胞 40 项目
- 癌细胞及细胞系 116 项目
- 白细胞单采样本 1 项目
- 白血病/淋巴瘤细胞 8 项目
- 真皮细胞 1 项目
- 神经元 136 项目
- 神经干/祖细胞 384 项目
- 神经细胞 2 项目
- 粒细胞及其亚群 61 项目
- 肝细胞 3 项目
- 肠道细胞 13 项目
- 肾脏细胞 2 项目
- 脑肿瘤干细胞 81 项目
- 血小板 1 项目
- 血浆 3 项目
- 调节性细胞 7 项目
- 造血干/祖细胞 779 项目
- 间充质干/祖细胞 133 项目
- 髓系细胞 99 项目
Show More
Show Less
研究领域
种属
- Mouse
Show More
Show Less


 EasySep™小鼠TIL(CD45)正选试剂盒
EasySep™小鼠TIL(CD45)正选试剂盒



 沪公网安备31010102008431号
沪公网安备31010102008431号