Hematopoietic Stem and Progenitor Cells (HSPCs): Isolation, Culture, and Assays
Hematopoietic Stem and Progenitor Cells (HSPCs): Isolation, Culture, and Assays
- Document # 29068
- Version 2.0.0
- 11/1/24
Introduction
Most blood cells have a finite lifespan and are replaced throughout life by the proliferation and differentiation of a very small population of pluripotent hematopoietic stem cells (HSCs). HSCs make up a very small population of the hematopoietic system, however, these cells possess the unique ability to self-renew and undergo successive stages of differentiation, ultimately giving rise to mature blood cells (Figure 1). Also making up a part of the hematopoietic system are short-term repopulating progenitor cells, which give rise to lineage-specific cell types. Collectively, these are referred to as hematopoietic stem and progenitor cells (HSPCs).
The bone marrow (BM) is the primary site of hematopoiesis in humans after birth. Certain treatments, such as cytokine administration (notably granulocyte colony-stimulating factor; G-CSF), myelosuppressive drugs used in cancer therapy, and agents disrupting hematopoietic-BM stromal cell interactions, facilitate rapid mobilization of stem and progenitor cells into circulation. Transplantation of BM or mobilized peripheral blood (mPB) from HLA-matched donors is a well-established therapy for leukemia and various hematologic and immune disorders. Moreover, umbilical cord blood (CB) obtained at birth and cryopreserved provides an alternative source of HSPCs, particularly for patients without suitable BM or mPB donors. Read more about the different sources of HSPCs here.
Recent technological advances in maintaining or amplifying HSPC populations in culture, alongside CRISPR/Cas9 gene editing techniques, have catalyzed the emergence of innovative cell and gene therapy approaches to treat genetic blood disorders like sickle cell disease and thalassemia. The development of cell and gene therapy applications depends on the progress of fundamental research into HSPC biology, predominantly explored through murine models, and the refinement of methodologies for HSPC identification, isolation, and functional characterization from diverse tissue sources, such as bone marrow, blood, and other tissues.
This review aims to provide a comprehensive overview of transplantation and culture assays devised to evaluate the hematopoietic potential of HSPCs. It further delves into phenotypic markers and methodologies for isolating mouse and human HSPCs. Additionally, the review explores culture systems tailored to expand limited HSPC pools in clinical grafts, promote HSPC proliferation and lineage-specific differentiation toward mature blood cell lineages, and generate HSPCs and blood cells from pluripotent stem cells (PSCs).
In Vivo Assays for Hematopoietic Stem and Progenitor Cells
An important characteristic of an HSC lies in its ability to restore blood cell production after transplantation. Experimental designs involving the transplantation of BM cells or purified HSPC subsets in mice have proven invaluable for understanding the biology of both mouse and human stem cells.
Transplantation Studies Using Mouse Cells
To assess the hematopoietic potential of mouse HSCs, BM cells are typically injected into mice whose hematopoiesis has been suppressed, commonly through irradiation. The subsequent repopulation of recipient mice with cells derived from the donor is monitored periodically in blood samples to examine repopulation kinetics. Furthermore, after a minimum of four months, donor-derived cells are evaluated in various tissues including BM, spleen, blood, and thymus to ascertain long-term engraftment (Szilvassy et al., 2002).
The transplantation assay format varies in the genetic backgrounds of donor and host mouse strains, the methodology employed to ablate or suppress hematopoiesis in the recipient pre-transplantation, the detection techniques utilized to identify the progeny of donor-derived stem cells, and the defined endpoints and criteria for determining "successful" engraftment.
In one type of assay, recipient mice undergo total body irradiation to eliminate HSPCs. Subsequently, these mice receive intravenous injections of BM cells or purified HSPCs from a donor mouse, along with "competitor" cells from the same mouse strain as the recipient mice (Purton et al., 2000). These competitor cells serve multiple purposes: providing short-term radioprotection, ensuring recipient survival, and exerting selective pressure to identify stem cells with robust competitive repopulating potential. Alternatively, other assays utilize recipient mice with defective endogenous hematopoiesis due to mutations in the Kit gene. In these models, transplantation with donor cells from wild-type mice is feasible without the need for co-transplanted radioprotective cells (Miller & Eaves, 1997).
The prevalent method for tracing the progeny of transplanted HSCs involves using donor and recipient mouse strains expressing different isoforms of the pan-leukocyte antigen CD45 (CD45.1 or CD45.2). This distinction enables the differentiation between donor and recipient cells via flow cytometry (Spangrude et al., 1988). While this technique effectively identifies donor-derived lymphocytes, granulocytes, monocytes, and HSPCs, it cannot detect donor-derived erythrocytes and platelets, as these cells lack CD45 expression. However, by employing transgenic donor cells expressing a readily detectable reporter molecule, such as green fluorescent protein (GFP), in all blood cell lineages, including the erythroid lineage, the engraftment of transplanted cells can be quantified across all cellular lineages (Boyer et al., 2019).
In this experimental setup, different cohorts of mice receive varying quantities of donor cells. After several months, the extent of hematopoietic reconstitution in each group of mice is evaluated. Utilizing Poisson statistics, researchers can then determine the frequency of repopulating cells within the transplanted cell population (Szilvassy et al., 1990). This methodology, complemented by single-cell transplantations wherein purified HSPCs are individually injected into groups of mice, facilitates a detailed quantitative analysis of HSC frequencies across diverse purified HSPC subsets. Moreover, it enables the investigation of engraftment dynamics and differentiation potential at the individual HSPC level. To investigate the in vivo self-renewal capacity of mouse HSCs, researchers can also perform serial transplantations, wherein bone marrow cells from primary recipients are transplanted into secondary, tertiary, and even quaternary recipients.
Recent advancements have revolutionized the study of HSCs by enabling the labeling of millions of individual cells within a heterogeneous population with unique genetic markers (“barcodes”). These markers, integrated into the genome, are inherited by subsequent generations of daughter cells. Upon transplantation of numerous tagged HSCs into recipient mice, the engraftment kinetics, size, and lineage distribution of each labeled HSC can be precisely quantified. This is achieved by identifying the specific barcode within blood cells using high-throughput parallel sequencing methods (Naik et al., 2014). This approach facilitates a comprehensive clonal analysis of multiple HSCs, overcoming the inherent limitations of traditional single-cell transplantation experiments.
Transplantation Studies Using Human Cells
The hematopoietic potential of human HSPCs can be investigated through transplantation into genetically immune-deficient mice, followed by the assessment of human blood cells in the blood, BM, or other organs of these mice several weeks to months later.
Traditionally, these assays were conducted using the severe combined immunodeficiency (SCID) and non-obese diabetic (NOD)/SCID mouse strains. However, these approaches required large cell numbers to overcome immune rejection by residual host macrophages and natural killer (NK) cells. Moreover, these assays exhibited a bias towards B-lymphocyte development, while impeding sustained long-term production of myeloid cells, platelets, and erythrocytes. Consequently, studying the kinetics of human cell engraftment or distinguishing between short-term and long-term reconstitution mediated by distinct HSC subsets was not possible.
The development of other immunodeficient mouse strains has alleviated many of these challenges. Specifically, β2-microglobulin-deficient and interleukin-2 receptor (IL-2R) γ-deficient NOD/SCID mice demonstrate robust engraftment levels for over 20 weeks post-transplantation (Cheung et al., 2013; Ito et al., 2002; Kollet et al., 2000; Shultz et al., 2005). IL-2Rγ-deficient mice, coupled with functional impairment of endogenous HSCs due to loss-of-function mutations in the Kit gene, exhibit even greater permissiveness for human HSC engraftment and prevent the need for pre-transplant conditioning via irradiation (Cosgun et al., 2014).
These enhanced xenotransplantation assays have facilitated a more comprehensive characterization of human HSCs and have been instrumental in studies identifying human HSCs at single-cell resolution (Notta et al., 2011). For further insights into the historical context of xenogeneic mouse transplantation assays and the utilization of other mouse strains, please refer to a recent review by Mian et al. (2021).
In Vitro Assays for Hematopoietic Progenitor Cells
While transplantation assays are essential for evaluating the engraftment potential and hematopoietic reconstitution ability of HSPCs in vivo, culture assays have also emerged as valuable tools for assessing the proliferative and differentiation capacities of these cells. These assays are capable of detecting hematopoietic cells at various stages of differentiation, ranging from multipotent progenitors to lineage-restricted progenitor cells. In the subsequent sections, we will delve into the principles and applications of two of the best-characterized culture assays, the colony-forming unit (CFU) assay and the long-term culture-initiating (LTC-IC) assay.

Figure 1. Hematopoietic Hierarchy, Assays and Markers in Mice and Humans
Schematic representation of the hematopoietic hierarchy from HSCs, via intermediate progenitor stages, to mature blood cells. Assays to identify HSCs and progenitors are shown at the top. The most definitive phenotypical markers used to identify the various types of mouse and human hematopoietic cells are shown at the bottom. Additional markers can be used to further distinguish between subsets. Refer to the text for further details. It should be noted that this model is continuously being revised and updated and several other ways of presenting the hematopoietic hierarchy and differentiation trajectories have been proposed (Laurenti & Gottgens, 2018). For example, HSCs are more heterogeneous with respect to self-renewal and differentiation abilities, and lineage commitment and differentiation are more continuous than suggested by surface marker expression profiles and functional criteria alone. The model also doesn't show the vast differences in the numbers of individual types of blood cells generated, with erythrocytes and neutrophils representing ~97% of the ~300 billion new blood cells (excluding platelets) produced in the human bone marrow every day under steady-state conditions. (Sender & Milo, 2021).
LT-HSC: Long-Term Hematopoietic Stem Cell; ST-HSC: Short-Term Hematopoietic Stem Cell; MPP: Multipotential Progenitor; CMP: Common Myeloid Progenitor; CLP: Common Lymphoid Progenitor; CFU-GEMM: Colony-Forming Unit – Granulocyte/Erythrocyte/Macrophage/Megakaryocyte; BFU-E: Burst-Forming Unit – Erythroid; CFU-E: Colony-Forming Unit – Erythroid; CFU-Mk: Colony-Forming Unit – Megakaryocyte; CFU-GM: Colony-Forming Unit – Granulocyte/Macrophage; CFU-G: Colony-Forming Unit –Granulocyte; CFU-M: Colony-Forming Unit – Macrophage
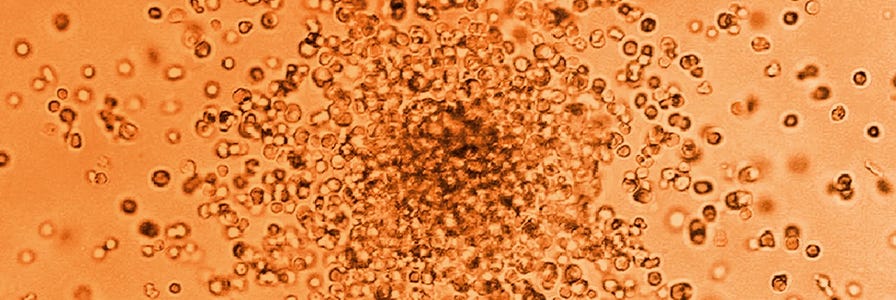
Colony-Forming Unit Assays
Since its inception over five decades ago (Bradley & Metcalf, 1966), the colony-forming unit (CFU) assay, also called colony-forming cell (CFC) assay, has emerged as the gold standard in vitro functional assay for investigating hematopoietic progenitor cells. In the CFU assay, cells are cultured at low cell density in a semi-solid medium, typically methylcellulose-based (e.g. MethoCult™), and supplemented with appropriate cytokines. These conditions support the proliferation and differentiation of individual progenitor cells, or CFUs, which give rise to discrete colonies in usually one to two weeks of culture. Distinct colonies arising from various types of progenitor cells are identified and quantified based on the number and types of mature cells they contain, utilizing morphological and phenotypic criteria. The CFU assay is primarily employed to detect multipotential and lineage-restricted progenitors of the erythroid, granulocytic, and macrophage lineages. Moreover, megakaryocyte and B-lymphoid progenitors can also be identified by applying selective culture conditions tailored to these specific cell types.
Widely utilized across research and clinical settings, the CFU assay is an important tool for examining the impacts of stimulatory and inhibitory agents on HSPC proliferation and differentiation, including potential toxicities of new drugs. Learn more in our whitepaper, The CFU Assay in Preclinical Toxicity Testing. Additionally, it facilitates the evaluation of in vitro manipulations, such as cell processing, cryopreservation, genetic modification, and ex vivo expansion culture, thereby ensuring the quality of cellular products utilized in hematopoietic cell transplantation and other therapeutic interventions.
Multiple studies have linked CFU counts to key transplantation outcomes, such as engraftment time and overall survival post-transplantation (Hogge et al., 2000; Iori et al., 2004; Page et al., 2011; Prasad et al., 2008; Yang et al., 2005; Yoo et al., 2007). Consequently, this assay is valuable for predicting graft quality, notably aiding in selecting cord blood units with viable progenitor cells before transplantation. Automated imaging platforms, such as STEMvision™, streamline colony counting, enhancing reproducibility and standardization (Velier et al., 2019).
Training: Introduction to STEMvision™ for Automated CFU Scoring
Learn how to standardize and automate the scoring of the CFU assay using STEMvision™ in this self-paced digital course. You’ll gain access to lectures, step-by-step protocol videos, and a library of curated resources.
Start Now >
Long-Term Culture Assay for Primitive Hematopoietic Progenitor Cells
The long-term culture (LTC) assay identifies more primitive progenitor cells than the CFU assay. The initial versions of the LTC assay developed in the late 1970s were designed to detect primitive progenitors of the myeloid (i.e. granulocyte, macrophage, erythroid, and megakaryocyte) lineages (Dexter et al., 1977; Gartner & Kaplan, 1980). Later advancements also facilitated the growth and identification of B lymphoid and NK cell progenitors (Miller et al., 1992; Whitlock & Witte, 1982).
In executing the LTC assay, hematopoietic cells are cultured atop an adherent monolayer derived from primary bone marrow or immortalized stromal cell lines. Using specialized culture media, such as MyeloCult™, this system fosters the survival, self-renewal, proliferation, and differentiation of primitive hematopoietic cells, including long-term repopulating HSCs, over extended periods spanning many weeks (Cho & Muller-Sieburg, 2000; Miller & Eaves, 2002).
The cells identified in LTC assays are termed long-term culture-initiating cells (LTC-ICs). These cells are typically distinguished by their ability to generate CFUs in the stroma-supported cultures for at least five weeks (four weeks for mouse cells). This duration ensures that any CFUs in the original cell sample undergo terminal differentiation. Consequently, CFUs detected after 4 - 5 weeks are newly generated from more primitive cells. The LTC-IC-derived CFUs are identified by re-plating the contents of individual cultures in CFU assay media (such as MethoCult™) and counting colonies approximately two weeks later (Miller & Eaves, 2002).
For optimal accuracy, LTC-IC assays ideally utilize a limiting-dilution design that enables measurement of the frequency of these progenitor cells. Alternatively, simple formats that measure the CFU output of bulk cultures can also determine the number of LTC-ICs if the CFU yield per LTC-IC is already established from prior studies. In a different iteration, individually purified primitive HSPCs are sorted into microwells containing stromal cells and culture medium. The clonal lineage output is assessed six weeks later (Knapp et al., 2018).
Markers and Methods for HPSC Isolation
In addition to the functional assays described in the previous paragraphs, HSPCs can also be distinguished based on their phenotype. This involves staining cells, typically with fluorescently labeled antibodies targeting cell surface antigens or DNA dyes, and subsequently analyzing through flow cytometry or microscopy. This method has greatly enhanced our understanding of key markers distinguishing HSCs, progenitors, and mature blood cells. Such insights have been essential for devising strategies to isolate HSCs from bone marrow (BM), blood, and other heterogeneous cell populations.
This section will delve into the most commonly utilized markers for identifying and purifying HSCs in mice and humans. Additionally, a summary detailing additional markers utilized to differentiate progenitor subsets, including common myeloid progenitors, common lymphoid progenitors, granulocyte and macrophage progenitors, and megakaryocyte and erythroid progenitors, was previously provided in Figure 1.
Mouse Cells
The initial step in identifying and isolating mouse HSPCs in BM, spleen, fetal liver, or other tissues usually involves the elimination of mature cells that express “lineage" (Lin) antigens specific to terminally differentiated blood cells. Lin antigens, such as CD3 for T cells, B220 for B cells and NK cells, Ly6G/Gr-1 for granulocytes, CD11b/Mac-1 for monocytes and macrophages, and TER-119 for erythroid cells, are absent or expressed weakly on HSPCs.
Following the elimination of lineage-positive (Lin+) cells through immunomagnetic isolation methods like EasySep™, HSPCs can be further characterized using combinations of cell surface markers, notably KIT (i.e. the receptor for stem cell factor [SCF], also known as CD117) and SCA1 (Muller-Sieburg et al., 1986; Okada et al., 1992; Osawa et al., 1996; Spangrude et al., 1988; Uchida et al., 2003).
Lin-SCA1+KIT+ (LSK) cells account for less than 0.1% of nucleated BM cells but contain most repopulating HSCs. However, SCA1 is only useful in some mouse strains (e.g. C57Bl/6), but not in BALB/c and other mouse strains which exhibit low SCA1 expression on HSCs (Spangrude & Brooks, 1992, 1993). Alternatively, markers and isolation strategies based on a Lin-CD48-CD150+ phenotype (the SLAM phenotype) are effective across most mouse strains (Kiel et al., 2005).
LSK and SLAM cells represent heterogeneous populations, with HSCs accounting for at most 10 - 20% of all cells. Further enrichment of HSCs, achieving frequencies as high as 50%, has been accomplished by selecting LSK or SLAM cells expressing elevated levels of CD201 (endothelial protein C receptor; EPCR) and low or undetectable levels of CD34, CD135 (FLT3), and CD49b. These enriched HSC populations retain low levels of DNA dyes like Rhodamine-123 (Rho123) and Hoechst 33342 due to the high expression of multidrug transporter proteins MDR1 and ABCG2, respectively (Balazs et al., 2006; Benveniste et al., 2010; Kent et al., 2009; Kiel et al., 2005; Osawa et al., 1996; Uchida et al., 2003; Uchida & Weissman, 1992).
Human HSPCs
The cell surface protein CD34 is the most important marker of primitive human hematopoietic cells. CD34 is expressed in 1 - 5% of nucleated human BM cells, approximately 1% of CB cells, and less than 0.1% of normal peripheral blood (PB) cells. Most human HSCs are CD34+, as demonstrated by xenotransplantation assays described above and clinical transplants performed with purified CD34⁺ cells from BM and mPB (Civin et al., 1996; Larochelle et al., 1996; Vogel et al., 2000) The CD34⁺ population also includes most LTC-ICs, CFU-GEMM, BFU-E, and CFU-GM. As cells differentiate, CD34 expression decreases, and the majority of late-stage progenitors (e.g. CFU-E) and mature blood cells become CD34- (Civin et al., 1996; Strauss et al., 1986).
CD34+ cells are enriched 50 to 200-fold by depleting Lin+ cells using methods such as EasySep™, RosetteSep™, or fluorescence-activated cell sorting (FACS). CD34 is expressed on approximately 40 - 90% of Lin- BM cells depending on the individual sample and experimental conditions, and can be further purified using CD34+ isolation methods. HSCs and primitive progenitors that are detectable in xenotransplantation and LTC-IC assays account for only 0.1 - 1% of CD34+ blood or BM cells, while progenitor cells that are detectable in CFU assays comprise about 10 - 30% of CD34+ cells. Therefore, CD34 expression alone is not sufficient to measure HSCs, and additional markers are required to identify and isolate the most primitive hematopoietic cells.
The most common markers to subfractionale CD34+ cells include CD38 and CD45RA, which are absent or only weakly expressed on primitive cells, and CD90 (THY1), which is expressed at higher levels on primitive cells than on differentiated cells (Craig et al., 1993; Lansdorp et al., 1990; Terstappen et al., 1991). As few as 10 Lin-CD34+CD38-CD45RA-CD90+ CB cells can engraft the BM of immunodeficient mice and generate human lymphoid and myeloid cells for at least 12 weeks after transplantation. These results demonstrate that Lin-CD34+CD38-CD45RA-CD90+ cells are highly enriched for long-term repopulating cells. Some CD90- cells can also engraft but at a lower level, and may represent a less primitive HSC subset than their CD90⁺ counterparts (Majeti et al., 2007).
A subset of Lin-CD34+CD38-CD45RA- also express the adhesion molecule CD49f and weakly retain the DNA dye, Rhodamine (Rho)-123 (Notta et al., 2011). In single-cell transplantation studies, close to 30% of the Lin-CD34+CD38-CD45RA-CD90+CD49f+Rho- low exhibited long-term multi-lineage repopulating ability (Notta et al., 2011). A similarly high HSC frequency of 1 out of 3 cells has been observed in limiting dilution transplantation experiments with purified CD34+CD38-CD45RA-EPCR+ cells. These cells are heterogeneous for CD90 expression, but nearly all are CD49f+ (Anjos-Afonso et al., 2022).
Human HSPCs can also be identified by measuring the activity of the intracellular enzyme aldehyde hydrogenase (ALDH), specifically the ALDH1a1 isozyme, which is involved in retinoid signaling and detoxification of aldehydes (Wang et al., 2022). ALDH converts a non-charged fluorescent substrate (ALDEFLUOR™), which passively crosses cell membranes, into a negatively charged polar fluorescent product, which cannot cross cell membranes and accumulates inside viable, intact ALDH-expressing cells. As a result, cells with high ALDH activity can be detected and isolated by flow cytometry based on their bright fluorescence (Storms et al., 1999). Both long- and short-term repopulating HSCs and most progenitor cells, with the possible exception of lymphoid progenitors, express high levels of ALDH (Hess et al., 2004; Storms et al., 2005). Flow cytometric methods to measure the frequency of CD34brightALDH-bright cells have been developed as a potency assay to measure the quality of CB units intended for transplantation (Shoulars et al., 2016).
The aforementioned markers and isolation strategies are vital for the isolation of HSPCs from diverse cell populations such as BM, mPB, or CB. Apart from CD38, which is primarily useful for distinguishing primitive and differentiated cells in noncultured cells, these markers play a crucial role in identifying HSPCs in cell culture experiments. In the subsequent section, we will explore various examples of HSPC culture methods. These encompass techniques aimed at (i) augmenting the limited numbers of HSPCs in grafts; (ii) activating HSPCs for gene editing purposes; (iii) generating mature blood cells in lineage-specific CD34+ cell cultures; and (iv) inducing hemogenic specification and differentiation of pluripotent stem cells to produce lineage-specific progenitor cells and mature blood cells.


 EasySep™小鼠TIL(CD45)正选试剂盒
EasySep™小鼠TIL(CD45)正选试剂盒






 沪公网安备31010102008431号
沪公网安备31010102008431号